If your doctor told you that your vitamin D is low, is your chance of getting COVID-19 greater? Or if you get COVID-19, are you more likely to get really sick or even die? Or will you respond less well to the vaccine—which I hope you’ve gotten by now? And if the answer to any of those questions is definitively yes, does that mean taking vitamin D supplements will help? That’s at least what a lot of the media would like you to believe, it seems.
If you get nothing else out of reading this blog, please understand and grudgingly accept 3 things:
- The answer to all those questions is, “We don’t know for sure, but probably not!”
- Just because a vitamin plays certain roles in your body to keep you healthy, it doesn’t mean taking a supplement of that vitamin will make you healthier. Sometimes it will actually make you sick (If you’re confused, I understand, but keep reading and all will be revealed, I hope!).
- Vitamin D, as nutrients go, is exceptionally complicated…and so is the human immune system.
I’ve spent the past year reading a lot of online nutrition advice, especially everything I can find on COVID-19 and nutrition. Why? Because when the public experiences a health crisis, there’s a tendency for people to reach out for anything that might work, and I’m no exception: Especially when the risks (by risks, I mean financial costs and side effects) don’t significantly outweigh the danger of becoming infected by the thing we’re trying to treat/prevent. Such “reaching out” can lead to people doing some pretty extreme things, nutritionally and otherwise. With my background I was hoping I could learn enough to help prevent people from spending money on something that would do nothing to help or, worse, actually cause themselves more problems!
Since the media love to present answers to complicated things in 20-second “sound-bites,” it didn’t surprise me at all that they would light up over the possibility that Vitamin D might help prevent COVID-19 or make it less severe. No, I’m not a psychic. There’s a reason they focused on vitamin D. Unlike most other nutrients—especially the ones with calories (protein, fat, and carbohydrates)—vitamin D insufficiency ( a mild decrease from normal levels) might actually be a real thing for many people in the United States, especially in the northern states. Why did I say “insufficiency?” Why the North? And is this a big deal? Please keep reading.
Why me?
Before I try to answer these questions, I’ll just briefly say that a few years ago, I helped lead a big study to review the scientific evidence for everything that vitamin D supplements do, which required also reviewing everything that we know vitamin D does in the body, what happens if we don’t have enough, and what “not enough” even means. Our study verified that the only real evidence for a role for vitamin D was in helping bones develop and grow; the evidence for any other potential role—like helping prevent cancer or heart disease—was just weak or non-existent. Then, this past year, I was asked to serve as a peer reviewer for a paper submitted to an online medical journal on the effects of several vitamins and minerals on your chances of getting an upper respiratory infection, most of which are caused by viruses. I knew the authors could not have looked specifically at effects of nutrients on COVID-19 because the data on COVID-19 were still too new to have been published in peer-reviewed journals, and this paper was a review of peer-reviewed studies. So I was kind of stunned to see that the authors still tried to extrapolate their findings regarding the other viruses to COVID-19! And if the authors were allowed to do this, imagine what it would do to the sales of vitamin and mineral supplements! But the overzealous overinterpretation of unreviewed, unpublished data that COVID has encouraged is a story for another time. The paper I evaluated—which I can now talk about because it’s been published—actually reviewed dozens of other people’s studies, some dating back decades, and not just on vitamin D but also on vitamin C, zinc (a required mineral), and multivitamins (so really the kitchen sink of supplements and studies) and their effects on upper respiratory infections. The study found that the results of existing studies are really too weak to support taking any particular vitamins or minerals to prevent or treat upper respiratory infections, although they tried to put a rosy spin on it. As a result of my evaluation, the editor of the journal asked me to write an editorial about the study (no good deed goes unpunished!). The editorial I wrote was about why the study revealed less about the effects of these nutrients on developing or surviving respiratory infections than it revealed about the poor state of much nutrition research and that the evidence certainly was not strong enough to support throwing nutrients at COVID-19. That was a long-winded way of saying, based on the vitamin and mineral research I’ve done over the past few years, I’m asked to answer these questions a lot.
Vitamin D Insufficiency, and “North to Alaska” IS a Big Deal!
What does Vitamin D do in the body, or what happens if we’re truly deficient? Although we know that vitamin D, like all vitamins, is involved in many processes in the body, the process that is most affected by deficiency (meaning the most visible one and the one we have the strongest evidence about, as I mentioned above), is bone growth, because one of the major jobs of vitamin D is to allow the body to properly use calcium to build bone. Infants and children who are severely deficient in vitamin D fail to experience normal bone growth and develop a disease called Rickets—a failure of normal skeletal development, nearly unheard of in the US since maybe the early 1900s (my grandfather, who was born in the late 1800s in heavily polluted Liverpool UK, had it). Our bones, in addition to keeping us from being formless blobs of flesh and organs, serve as a giant pantry for calcium, a mineral critically needed by every cell in our bodies to keep working and prevent death. So, because our bones continue to reform themselves throughout our lives, adults who are severely deficient in vitamin D or calcium can also experience bone problems. Because of this big, well-understood vitamin D-bone connection, the Food and Nutrition Board of the National Academy of Sciences has based its recommendations for vitamin D intake on how much is needed to support normal bone development.
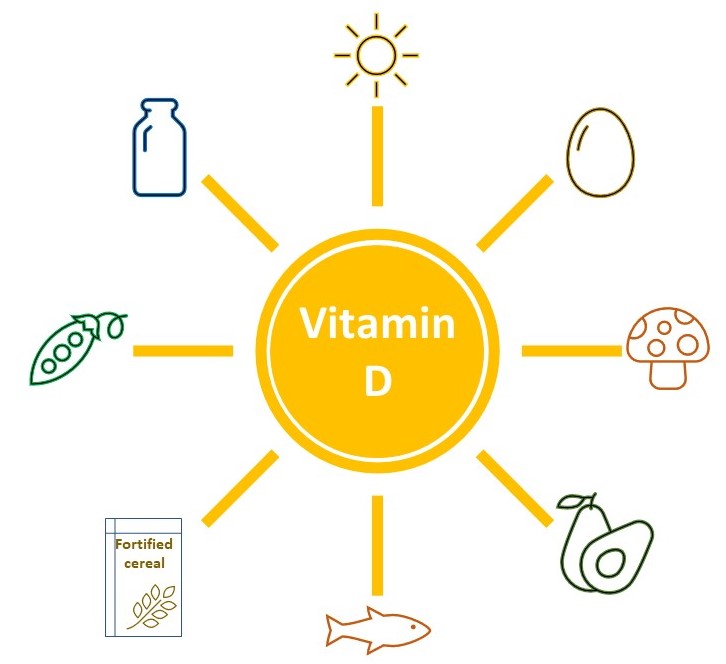
Now, let me throw a monkey wrench into the works: Not getting enough vitamin D isn’t only caused by poor diet—in fact it’s actually a challenge to get enough vitamin D from the foods most of us eat. We mainly get vitamin D by being outdoors in sunlight. Huh? Our bodies actually make an inactive form of vitamin D that is activated by the exposure of our skin to sunlight. So serious pollution (which can filter the needed rays of sunlight), fear of skin cancer (which keeps us indoors or shrouded like mummies when we go out), or even living in the northern US (so Alaska, for example) can reduce our vitamin D levels. This is why the vitamin D levels in our bodies change with the seasons and depend on where we live and what we do all day. And this has complicated the job of nutrition experts who are trying to determine how much vitamin D we should consume through foods (like fish and fortified milk); how much we can expect to make, given our relative lack of sun exposure; what really constitutes deficiency or insufficiency (this is the scientific term used to describe a mild deficiency); and when it would be appropriate to take supplements. Vitamin D is exceptionally complicated!
The immune system and its complexities
Let me start to tie this in with the immune system. As I said, vitamin D has a lot of functions in the body. Some studies have shown that it might help strengthen our immune systems: those organs and cells that fight infection by recognizing and attacking foreign invaders. All nutrients play some role in the function of our immune systems, which is why malnourished individuals are more prone to infections, especially infections of the digestive tract, which in turn worsens their nutritional status. However, improving our bodies’ ability to fight infection—boosting our immune function—is not so easy. It’s actually a complex problem that has eluded scientists, despite huge investments of time and effort.
Much about the immune system remains a complete mystery. For example, allergies are a form of immune system hyperactivity that serves no useful purpose and can even be lethal. Likewise, autoimmune diseases (e.g., Rheumatoid Arthritis or Celiac disease), in which the immune system becomes overactive and begins to attack parts of the body, offer no encouragement for boosting our immune systems and actually often require immune suppression!
So given what we know and don’t know about immune function, trying to determine which nutrients might play a special role in the function of our immune systems (so we can pop a few supplements to boost immunity) gets really tricky. For example, despite the plethora of ads you’ve probably seen for antioxidant supplements to improve immune function, one of the largest studies of antioxidant supplements ever conducted—in Finnish men who were smokers—actually found that the supplements increased death rates!
Back to Vitamin D and its complexities
To heap even more confusion on this already confusing area, here are a few more things we don’t quite understand about vitamin D. Sometime in the late 20th century, researchers began to suspect that the test they used to measure vitamin D in our blood was inaccurate and replaced it with a seemingly more accurate test. This meant that new test data can’t be compared or combined with data from studies that used the older test. It also means that individuals previously considered to have “sufficient” levels of vitamin D might now be considered to have vitamin D insufficiency—maybe not quite enough vitamin D but not enough of a drop to be considered truly deficient.
Furthermore, we still don’t really know whether what the current test is measuring is quite the right thing. A person might have blood levels of vitamin D that appear insufficient, while having levels (or chemical forms) elsewhere in the body that are perfectly sufficient but not easily measured—or vice versa. For the level of a nutrient that we can measure to be a useful measure—called a “marker”—that measure must be a perfect reflection of the stores (called pools) of that nutrient that the body draws from for important functions. So for example, we need the test for vitamin D status to be accurately measuring the adequacy of the pool of vitamin D being used to build bone. Remember in my last blog when I likened measuring blood levels of certain nutrients to the drunk looking for his car keys under the streetlight, because that’s where the light is best? For over a decade, an international body of experts has been trying to determine what form(s) of vitamin D should be measured, in what part of the body, and how to measure them most accurately. And in fact, if your health care providers haven’t routinely measured your vitamin D levels, you should congratulate them! The United States Preventive Services Task Force, an independent board of world-renowned experts, has recently reviewed the literature and determined that there is no benefit to routinely screening people for Vitamin D deficiency. Why? Please read on.
When people get sick, their doctors often run blood tests, and it’s not unusual to find their blood levels of vitamin D are low. This makes total sense, and as I provide my rationale, please look back to my “monkey-wrench” paragraph if necessary. Like all vitamins and minerals, vitamin D is being used up to fight the illness. When we’re sick, we’re often not eating well, nor are we spending time outdoors. Therefore, it’s not at all surprising our vitamin D levels might be low when we get sick. Since no one actually knows what any particular person’s normal levels of vitamin D are or should be (because remember: season and place of residence—see “monkey wrench” above!), it’s impossible to interpret a single measurement of vitamin D in someone who’s not feeling well. And actually, the same thing applies even to someone who’s feeling fine, because, again, studies of healthy people have shown widely varying levels of vitamin D. Almost no studies of the effects of Vitamin D on the risk for upper respiratory infections measured people’s nutrient levels before or even after giving them vitamin D, so if people who got vitamin D supplements got sick less, it was impossible to know if Vitamin D had anything to do with these better outcomes. And if they got sick in spite of getting vitamin D, does that mean their levels of vitamin D were just super low to begin with? Was the study long enough or the doses large enough for the vitamin D to have had any effect? Would supplements even have helped increase the pools of vitamin D in the body that the immune system needs to draw on? Or, as is often the case in developing countries, could these people have been deficient in multiple nutrients, so that any possible benefit vitamin D might have had was masked or prevented? These are important questions, not just with studies of vitamin D, but with much of the research on individual nutrients.
Vitamin D and COVID-19
With all that in mind, let’s now get to COVID-19! The reason “snake-oil” salesmen are so popular is that they promise a quick fix for a problem no one else has been able to solve. What seems hard to grasp is that the research needed to find real solutions can take time, sometimes entire lifetimes, frustrating and overwhelming those of us just looking to improve our health. (It’s no wonder some “experts” who should know better are attaining extreme financial success by touting things like “green coffee bean extract” as a “magical diet ingredient” with no credible scientific data to back it up, but that’s for another time)!
So far, about three different kinds of studies have been used to try to figure out whether Vitamin D is beneficial for people with COVID-19. I’m being generous by calling these studies because for the most part, they’re just collections of observations about people who got COVID-19, and usually people who were sick enough to require hospitalization.
- The first has asked whether COVID-19 patients tend to be vitamin D insufficient or even deficient. Yes, many people with COVID-19 have low levels of vitamin D: If this seems like a surprise, please go back and reread the previous section. But were they insufficient (or deficient) before they got sick? This is an important piece of the puzzle, but of course there is no way to find out with studies like this, called observational studies.
- Regardless, the observation of low vitamin D levels in many COVID-19 patients drove some members of the health care community to think Vitamin D supplements were worth a try, so in the second kind of study, doctors just started giving vitamin D to COVID-19 patients, sometimes injections of “megadoses,” to see if Vitamin D would help prevent hospitalization, shorten hospital stays, or prevent death. These studies have mostly shown no effect of vitamin D. And studies that have shown a beneficial effect of vitamin D are next to impossible to interpret, given the highly varied course of COVID-19 from one person to the next, meaning that one person feels fine within a week or two while the next person ends up in the ICU. We just don’t know which, if any, of those patients would have gotten better faster—or remained less sick—on their own, without getting any vitamin D. And to complicate our interpretation of the studies further, most of the patients were also getting other treatments at the same time. Yikes!!!
- Finally, some researchers gave apparently healthy people vitamin D supplements and—hopefully—compared their chances of getting COVID-19 with the chances of people who didn’t get supplements. Again, results were mostly discouraging. But without knowing these people’s initial vitamin D levels, with more and more people getting the vaccine, and the decreasing risk of getting COVID-19, it is unlikely we will learn anything useful about whether vitamin D prevents COVID-19.
So, at this point, there are really no definitive answers to whether taking vitamin D supplements can help prevent COVID-19, but it doesn’t look promising. And if you’re asking why not just take the vitamin anyway? What could go wrong? Well, some things could! Taking excessive amounts of vitamin D supplements is not safe: It can cause large amounts of calcium to move from your bones into your bloodstream, a condition called hypercalcemia (hyper=excess, calc=calcium, emia=in your blood), which can cause nausea, vomiting, weakness, confusion, and eventually, kidney and bone damage. Since we now have vaccines that work, let’s all just root for evidence-based scientific research. If you’re asking, ”Will vitamin D help vaccines work better?” the answer is the same—we don’t know, but probably not—for all the reasons I’ve laid out above.
Finally, if you’ve had your vitamin D levels measured and your health care provider has told you your vitamin D is low and advises you to take vitamin D supplements, it’s important to ask them to explain the test results and possibly even repeat the tests a few months later. And if repeated tests show you are truly deficient, make sure you’re taking a supplement that carries the USP Verified label, never take more than the recommended amount, consume some of your vitamin D in food, and try to step outdoors, even for 10 minutes a day.
In my next few blogs, I’m going to cover less controversial things, like which diets work best(😉), is caffeine safe, and do probiotics work!